Safe Sex Practices for All: A Comprehensive Guide for Every Sexual Orientation

Key Takeaways
- Inclusive Practices: Safe sex practices must be tailored to accommodate the diverse needs of all sexual orientations, ensuring effectiveness and inclusivity.
- Comprehensive Protection: Utilizing a variety of protective measures, including condoms, dental dams, and lubricants, is essential in preventing sexually transmitted infections (STIs) and unintended pregnancies.
- Education and Awareness: Comprehensive sexual education that addresses the unique challenges faced by different sexual orientations enhances overall sexual health and wellness.
- Regular Health Check-ups: Routine STI screenings and sexual health check-ups are crucial for maintaining sexual wellness across all orientations.
- Integration with Sexual Wellness Tools: Incorporating sex toys and other sexual wellness products can enhance pleasure while adhering to safe sex practices.
Table of Contents
- Introduction
- Understanding Safe Sex
- Safe Sex Practices by Orientation
- Choosing the Right Protection
- Regular Health Check-ups and STI Testing
- Integrating Safe Sex with Sex Toys
- Overcoming Barriers to Safe Sex
- Case Studies and Statistics
- Visual Element: Comparison of Safe Sex Practices Across Orientations
- Comprehensive FAQ
- Conclusion
- References
Introduction
Safe sex practices are essential for maintaining sexual health, preventing the spread of sexually transmitted infections (STIs), and avoiding unintended pregnancies. These practices are crucial for individuals of all sexual orientations, including heterosexual, homosexual, bisexual, pansexual, and queer individuals. Understanding and implementing comprehensive safe sex strategies can significantly enhance sexual wellness and overall quality of life.
At sextoyforyou.store, we recognize the diverse needs of our clientele and are committed to providing inclusive resources and products that support safe and fulfilling sexual experiences. This comprehensive guide aims to educate individuals on safe sex practices tailored to their specific orientations, ensuring that everyone has access to the knowledge and tools necessary for maintaining sexual health. Whether you’re new to the concept of safe sex or looking to refine your practices, this guide offers in-depth information to empower your sexual wellness journey.
Sexual wellness is a multifaceted concept that encompasses physical, emotional, mental, and social well-being in relation to sexuality. It involves a positive and respectful approach to sexuality and sexual relationships, ensuring that individuals have the knowledge, resources, and tools necessary to achieve fulfilling and safe sexual experiences. Given the diversity in sexual orientations, it is essential to recognize and address the unique challenges and needs that different communities may face. This guide aims to provide an extensive overview of safe sex practices, emphasizing inclusivity and effectiveness across all orientations.

Understanding Safe Sex
Definition and Importance
Safe sex refers to sexual activities and practices that reduce the risk of transmitting or acquiring sexually transmitted infections (STIs) and prevent unintended pregnancies. It encompasses a range of protective measures, including the use of condoms, dental dams, and other barriers, as well as regular health check-ups and open communication between partners. Safe sex practices are not only about preventing diseases but also about fostering respectful and consensual sexual relationships.
The importance of safe sex cannot be overstated. According to the World Health Organization (WHO), there are over 1 million STIs acquired every day worldwide, with significant health, social, and economic consequences (WHO, 2023). Effective safe sex practices are crucial in mitigating these numbers, promoting individual health, and fostering responsible sexual behavior. By adopting safe sex practices, individuals can protect themselves and their partners from infections, maintain reproductive health, and enjoy more fulfilling and worry-free sexual relationships.
Moreover, safe sex practices contribute to reducing the stigma associated with STIs and promoting a culture of openness and responsibility. Educating oneself and others about safe sex is a proactive approach to sexual health that benefits individuals and communities alike.
Common Misconceptions

Despite widespread awareness campaigns, several misconceptions about safe sex persist, leading to inadequate protection and increased health risks:
- Condoms Reduce Pleasure: One of the most pervasive myths is that using condoms diminishes sexual pleasure. While it’s true that some individuals may perceive a slight reduction in sensation, modern condoms are designed to enhance pleasure. Innovations such as ultra-thin materials, textured surfaces, and lubricated varieties aim to maximize sensitivity and comfort, making condom use a pleasurable and safe addition to sexual activities (Smith & Duggan, 2013).
- STIs Only Affect Certain Orientations: There is a misconception that STIs are exclusive to specific sexual orientations. In reality, STIs can affect anyone, regardless of their sexual orientation. Misconceptions that STIs are limited to heterosexual or homosexual individuals can lead to inadequate protection and increased transmission rates. Comprehensive safe sex practices are essential for all, irrespective of their orientation (CDC, 2022).
- Oral Sex Is Completely Safe: While the risk of transmitting STIs through oral sex is generally lower compared to vaginal or anal sex, it is not entirely risk-free. Infections such as herpes, gonorrhea, and HPV can be transmitted through oral sex. Using barriers like dental dams can significantly reduce the risk of STI transmission during oral activities, ensuring safer practices (Plummer et al., 2013).
- Only Women Need to Worry About STIs: Another common misconception is that only women need to be concerned about STIs. Men can also acquire and transmit STIs, often without showing symptoms. Regular testing and protective measures are crucial for everyone involved in sexual activities to prevent the spread of infections.
- If You Feel Fine, You’re STI-Free: Many believe that if they feel healthy, they are free from STIs. However, many STIs are asymptomatic, meaning individuals can carry and transmit infections without showing any signs or symptoms. Regular screenings are essential for early detection and treatment, even if no symptoms are present (CDC, 2022).
Understanding and debunking these misconceptions is vital for promoting effective safe sex practices. Education and awareness campaigns play a crucial role in addressing these myths, ensuring that individuals make informed decisions about their sexual health.
Safe Sex Practices by Orientation
Safe sex practices must be tailored to accommodate the diverse needs of individuals across different sexual orientations. Each orientation may involve unique sexual activities and associated risks, necessitating specific protective measures and educational approaches. Below, we explore safe sex practices for heterosexual, homosexual, bisexual, pansexual, and queer individuals.
Heterosexual Individuals

Heterosexual individuals, engaging primarily in vaginal and sometimes anal intercourse, face specific safe sex challenges and considerations:
- Condom Use: Condoms are essential for preventing both STIs and unintended pregnancies. They act as a barrier, reducing the risk of transmitting infections like HIV, chlamydia, gonorrhea, and syphilis, while also serving as a reliable contraceptive method (Trussell, 2011). It is crucial to use condoms consistently and correctly every time you engage in vaginal or anal intercourse to maximize protection.
- Regular STI Testing: Routine screenings are vital, especially for sexually active individuals with multiple partners. Early detection and treatment of STIs can prevent complications and reduce transmission rates. Regular testing ensures that individuals are aware of their sexual health status and can take appropriate measures to protect themselves and their partners.
- Education on Contraception: Understanding different contraceptive methods empowers individuals to make informed choices about their reproductive health. Options include hormonal birth control (pills, patches, injections), intrauterine devices (IUDs), implants, and emergency contraception. Each method has its own set of benefits and considerations, and consulting with a healthcare provider can help determine the most suitable option (Trussell, 2011).
- Safe Sex Communication: Open and honest communication with partners about sexual history, STI testing, and contraceptive preferences is essential. Discussing these topics can lead to better understanding, mutual respect, and enhanced sexual satisfaction.
Homosexual and Bisexual Individuals

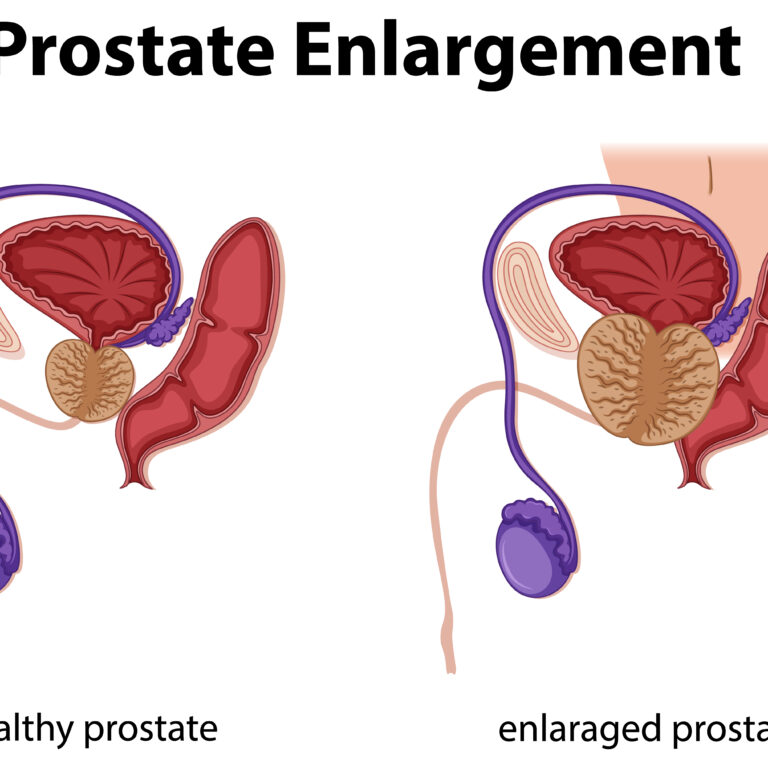
Homosexual and bisexual individuals, particularly men who have sex with men (MSM), encounter unique safe sex considerations due to the higher prevalence of certain STIs and specific sexual practices:
- Higher STI Risk: MSM are at a higher risk for STIs like HIV/AIDS, gonorrhea, syphilis, and hepatitis B. This increased risk is due to factors such as higher transmission rates during anal intercourse and the social dynamics within MSM communities that may influence sexual behavior (CDC, 2022).
- Use of Pre-exposure Prophylaxis (PrEP): PrEP is a medication taken daily to prevent HIV infection. Studies have shown that PrEP can reduce the risk of contracting HIV by up to 99% among individuals at high risk when taken consistently (Grant et al., 2010). PrEP is a critical preventive measure for MSM, especially those with multiple partners or those engaging in high-risk sexual activities.
- Regular STI Testing and Screening: Due to the higher risk of STIs, regular testing is crucial for MSM. Comprehensive screenings that include tests for HIV, gonorrhea, chlamydia, syphilis, and hepatitis are recommended. Early detection allows for timely treatment and reduces the likelihood of transmission to others.
- Targeted Prevention Methods: Implementing strategies such as post-exposure prophylaxis (PEP) after potential HIV exposure and using water-based lubricants to prevent condom breakage can enhance protection. Additionally, adopting safer sexual practices, such as reducing the number of sexual partners and avoiding high-risk activities, can further decrease STI risk.
- Community Support and Resources: Engaging with supportive communities and accessing resources tailored to MSM can provide valuable information and encouragement for maintaining sexual health. Organizations and online platforms offer education, counseling, and access to preventive measures like PrEP.
Queer and Pansexual Individuals

Queer and pansexual individuals, with their diverse sexual practices and attractions beyond the binary understanding of gender, require inclusive and adaptable safe sex strategies:
- Customized Protection: Utilizing a variety of protective barriers, such as condoms, dental dams, and gloves, depending on the type of sexual activity is essential. For instance, condoms can be used during penetrative sex, while dental dams are necessary for oral sex to prevent STI transmission (CDC, 2022).
- Inclusive Sexual Education: Access to education that acknowledges and addresses the specific needs of queer and pansexual individuals helps in adopting effective safe sex practices. Comprehensive sexual education should cover a wide range of topics, including diverse sexual orientations, gender identities, and the use of various protective measures.
- Supportive Communities and Networks: Engaging with supportive communities can provide access to resources, information, and encouragement for maintaining sexual health. These communities often offer safe spaces to discuss sexual health concerns, share experiences, and access tailored prevention strategies.
- Adaptable Protective Measures: Understanding that sexual practices can vary widely within queer and pansexual populations is crucial. Protective measures should be adaptable to accommodate different forms of sexual expression, ensuring that all individuals can engage in safe and enjoyable sexual activities.
- Mental Health and Sexual Health Integration: Addressing the intersection of mental health and sexual health is vital for queer and pansexual individuals. Stressors related to stigma, discrimination, and identity exploration can impact sexual wellness. Integrating mental health support with sexual health practices ensures a holistic approach to well-being.
By recognizing and addressing the unique safe sex needs of queer and pansexual individuals, we can promote a more inclusive and effective approach to sexual health that caters to all members of the LGBTQ+ community.
Choosing the Right Protection

Selecting the appropriate protective measures is fundamental to effective safe sex practices. The choice of protection depends on various factors, including the type of sexual activity, personal preferences, and any existing health conditions. Understanding the different types of condoms, barriers, lubricants, and other protective measures is essential for maintaining sexual health.
Types of Condoms and Barriers
Condoms and barriers are primary tools in safe sex practices, offering protection against STIs and unintended pregnancies. Understanding the different types available can help individuals choose the most suitable option for their needs:
- Condoms: Condoms are widely used for their dual protection against STIs and unintended pregnancies. They are available in various materials, each with its own set of benefits and considerations:
- Latex Condoms: The most common type, latex condoms are highly effective in preventing STI transmission and pregnancies. However, they are unsuitable for individuals with latex allergies (Mayo Clinic, 2021).
- Polyurethane Condoms: Made from a type of plastic, these condoms are suitable for individuals with latex allergies. They are thinner than latex condoms, offering enhanced sensitivity, but are less elastic, making them more prone to breakage if not used correctly (Mayo Clinic, 2021).
- Polyisoprene Condoms: These are another alternative for those with latex allergies. Polyisoprene condoms mimic the feel of latex without the allergens, providing a balance between sensitivity and strength (Mayo Clinic, 2021).
- Dental Dams: Dental dams are thin sheets of latex or polyurethane used during oral sex to create a barrier between the mouth and genital or anal areas. They prevent the transmission of STIs by blocking direct contact with bodily fluids. Dental dams are essential for safe oral sex practices, especially for individuals engaging in cunnilingus or anilingus (Plummer et al., 2013).
- Gloves: Latex or nitrile gloves can be used during manual stimulation to prevent the transmission of STIs. They provide a barrier between the hands and genital areas, reducing the risk of infection. Gloves are particularly useful for activities involving direct skin-to-skin contact or exchange of bodily fluids (CDC, 2022).
- Female Condoms: Also known as internal condoms, female condoms are inserted into the vagina or anus to provide a barrier against STIs and unintended pregnancies. They offer an alternative for individuals who prefer not to use male condoms and can be used by both men and women (Trussell, 2011).
Lubricants: Water-based vs. Silicone-based
Lubricants play a crucial role in enhancing comfort during sexual activities and preventing condom breakage. Choosing the right type of lubricant is essential for both safety and pleasure:
- Water-based Lubricants: These lubricants are versatile and compatible with all types of condoms and sex toys. They are easy to clean, non-staining, and generally safe for sensitive skin. However, they may require reapplication during extended use, as they tend to dry out more quickly than other types (Bailey et al., 2016).
- Silicone-based Lubricants: Silicone lubricants are long-lasting and water-resistant, making them ideal for activities like anal sex or use in water environments such as showers or hot tubs. They provide a silky smooth feel and do not dry out easily. However, they are not compatible with silicone sex toys, as they can degrade the material and reduce the toy’s lifespan (Plummer et al., 2013).
- Oil-based Lubricants: While oil-based lubricants can provide excellent glide and are often used for massage, they are not recommended for use with latex condoms, as they can cause the condoms to break. Oil-based lubricants are also harder to clean and can stain fabrics (CDC, 2022).
- Hybrid Lubricants: These lubricants combine the best qualities of water-based and silicone-based lubricants, offering long-lasting glide without damaging silicone sex toys. They provide a balance between ease of cleaning and durability, making them a popular choice for many individuals.
Choosing the right lubricant involves considering the type of sexual activity, any allergies or sensitivities, and compatibility with condoms or sex toys. Experimenting with different types can help individuals find the most suitable option for their preferences and needs.
Other Protective Measures

In addition to condoms and barriers, other protective measures can enhance safe sex practices and provide additional layers of protection:
- Dental Dams: As mentioned earlier, dental dams are essential for safe oral sex practices, preventing the transmission of STIs by blocking direct contact with bodily fluids. They are particularly useful for cunnilingus and anilingus, ensuring that both partners remain protected.
- Internal Barriers: Female condoms, also known as internal condoms, offer a protective barrier that is inserted into the vagina or anus. They are an alternative for individuals who prefer not to use male condoms and provide similar protection against STIs and unintended pregnancies (Trussell, 2011).
- Emergency Contraception: While not a primary preventive measure, emergency contraception can be used after unprotected sex to prevent unintended pregnancies. It is important to note that emergency contraception does not protect against STIs. Options include the morning-after pill and copper IUDs, which can be highly effective when used within a specific time frame after intercourse (Trussell, 2011).
- Pre-exposure Prophylaxis (PrEP): For individuals at high risk of HIV infection, PrEP is a preventive medication taken daily to significantly reduce the risk of contracting HIV. PrEP is highly effective when taken consistently and is an important component of a comprehensive safe sex strategy for those in high-risk groups (Grant et al., 2010).
- Post-exposure Prophylaxis (PEP): PEP involves taking antiretroviral medications within 72 hours of potential HIV exposure to prevent the virus from taking hold. It is not a substitute for regular prevention methods but can be a critical intervention in emergency situations (Grant et al., 2010).
Implementing a combination of these protective measures can provide comprehensive protection, enhancing overall sexual health and wellness.
Regular Health Check-ups and STI Testing

Regular health check-ups and STI testing are fundamental components of safe sex practices. They ensure early detection and treatment of infections, reducing the risk of complications and transmission to others. Understanding the importance of routine screenings, knowing how to approach healthcare providers, and utilizing resources for discreet testing are essential for maintaining sexual wellness.
Importance of Routine Screenings
Routine screenings for STIs are vital for sexually active individuals, regardless of their sexual orientation. Early detection of infections allows for timely treatment, preventing long-term health complications and reducing the likelihood of transmission to sexual partners. According to the Centers for Disease Control and Prevention (CDC, 2022), regular STI screenings are recommended for individuals with multiple sexual partners, those who engage in high-risk sexual activities, and individuals who have a history of STIs.
Routine screenings not only protect individual health but also contribute to public health efforts to control and reduce the spread of STIs. By staying informed about their sexual health status, individuals can make informed decisions about their sexual activities and take necessary precautions to protect themselves and their partners.
How to Approach Healthcare Providers
Approaching healthcare providers for sexual health concerns should be done with openness and honesty to ensure accurate diagnosis and effective treatment:
- Choose the Right Provider: Select a healthcare provider who is knowledgeable, respectful, and sensitive to diverse sexual orientations. Providers who are experienced in LGBTQ+ health issues can offer more tailored and empathetic care.
- Be Prepared: Before your appointment, consider what information you need to share. This may include details about your sexual history, number of partners, types of sexual activities, and any symptoms you may be experiencing. Being prepared can help facilitate a more productive and informative discussion.
- Confidentiality Assurance: Most healthcare providers ensure confidentiality, making it safe to discuss sensitive sexual health issues. Understanding your rights regarding privacy can alleviate concerns about sharing personal information.
- Ask Questions: Don’t hesitate to ask questions about your sexual health, STI testing procedures, and any concerns you may have. Seeking clarity on these topics can enhance your understanding and help you make informed decisions about your health.
Resources for Discreet Testing
For individuals seeking discreet STI testing, various resources are available to ensure privacy and convenience:
- Home Testing Kits: Home testing kits allow individuals to collect samples in the privacy of their own homes and send them to a laboratory for analysis. These kits provide a discreet and convenient way to monitor sexual health without the need for in-person visits (Plummer et al., 2013).
- Anonymous Clinics: Some clinics offer anonymous testing services where personal information is not required. These clinics provide a safe space for individuals to get tested without fear of judgment or exposure.
- Online Services: Platforms like sextoyforyou.store provide information and resources on obtaining discreet testing services. Online consultations and telehealth services can also offer confidential advice and referrals for STI testing.
- Local Health Departments: Many local health departments offer free or low-cost STI testing services. These services are often confidential and can be accessed without insurance.
Utilizing these resources ensures that individuals can maintain their sexual health discreetly and effectively, reducing barriers to regular testing and promoting overall wellness.
Integrating Safe Sex with Sex Toys
Sex toys can significantly enhance sexual wellness by providing additional stimulation, helping individuals explore their bodies, and facilitating communication between partners. However, integrating sex toys into sexual activities requires adherence to safe sex practices to prevent infections and ensure enjoyable experiences.
Cleaning and Maintenance of Sex Toys
Proper cleaning and maintenance of sex toys are essential to prevent infections and ensure their longevity. Neglecting to clean sex toys can lead to the buildup of bacteria, which can cause infections or other health issues.
- Material-Specific Cleaning: Different materials require different cleaning methods. For example:
- Silicone Toys: These can be boiled for a few minutes or washed thoroughly with soap and water. Silicone is non-porous, making it easy to sanitize.
- Latex and Rubber Toys: These should be hand-washed with mild soap and water. Avoid using harsh chemicals or abrasive cleaners, which can degrade the material.
- Stainless Steel and Glass Toys: These are non-porous and can be sterilized by boiling or using specialized toy cleaners.
- Storage Practices: Store sex toys in clean, dry places, preferably in individual pouches to prevent contamination and material degradation. Avoid storing toys in direct sunlight or extreme temperatures, which can damage certain materials.
- Regular Inspection: Periodically check sex toys for signs of wear and tear, such as cracks, discoloration, or changes in texture. Damaged toys should be repaired if possible or replaced to maintain safety.
Safe Use Practices to Prevent Infections
Implementing safe use practices can significantly reduce the risk of infections when using sex toys:
- Use Barriers: When sharing sex toys between partners, use condoms over the toy and change them between different types of sexual activities to prevent the transmission of STIs. This practice ensures that the barrier is effective in preventing direct contact with bodily fluids.
- Avoid Sharing Certain Toys: Toys that come into direct contact with bodily fluids, such as internal vibrators or dildos used for penetration, should not be shared unless thoroughly cleaned or used with barriers. Sharing these toys without protection increases the risk of STI transmission.
- Lubricant Compatibility: Ensure that the lubricant used is compatible with the sex toy material to prevent degradation and reduce the risk of irritation. For instance, avoid using oil-based lubricants with latex condoms, as they can cause the condom to break.
- Personal Use: Whenever possible, use sex toys for personal use to minimize the risk of cross-contamination. If sharing is desired, ensure that proper cleaning and barrier methods are employed.
- Regular Replacement: Replace sex toys that show signs of wear and tear or have been in use for an extended period. Regularly updating sex toys ensures that they remain safe and effective for use.
Recommended Products from sextoyforyou.store
At sextoyforyou.store, we offer a wide range of sex toys designed with safety and inclusivity in mind. Our products are crafted from high-quality materials, ensuring durability and ease of maintenance. Here are some of our recommended products that align with safe sex practices:
- Condom-Compatible Toys: Products made from materials like silicone and stainless steel that are safe to use with condoms and easy to clean. These toys provide versatility and safety, allowing for various sexual activities without compromising protection (sextoyforyou.store).
- Barrier Accessories: We offer dental dams, glove packs, and condom applicators to enhance safe sex practices. These accessories are essential for preventing STI transmission during oral sex and manual stimulation, ensuring a safer and more enjoyable experience (sextoyforyou.store).
- Hygienic Storage Solutions: Our selection includes individual pouches and storage cases to keep your toys clean and protected. Proper storage helps maintain the integrity of sex toys, preventing contamination and prolonging their lifespan (sextoyforyou.store).
- Versatile Lubricants: We provide a variety of lubricants, including water-based and silicone-based options, to complement your sex toys and enhance comfort during sexual activities. Our lubricants are designed to be compatible with a wide range of materials, ensuring safety and pleasure (sextoyforyou.store).
By selecting high-quality, safe sex toys from our collection, you can enjoy enhanced pleasure while maintaining your sexual health. Our products are thoughtfully designed to meet the diverse needs of our clientele, promoting a fulfilling and healthy sexual life.
Overcoming Barriers to Safe Sex
Adopting safe sex practices can be challenging due to various barriers, including stigma, lack of education, and societal pressures. Overcoming these barriers is essential for promoting sexual wellness and ensuring that individuals can engage in safe and fulfilling sexual activities.
Addressing Stigma and Shame
Stigma and shame surrounding sexual health and safe sex practices can hinder individuals from adopting protective measures and seeking necessary resources. Addressing these negative emotions involves fostering a culture of openness and acceptance:
- Educational Campaigns: Increasing awareness and education about the importance of safe sex can help reduce stigma and normalize protective behaviors. Educational initiatives should focus on demystifying sexual health topics and emphasizing the importance of prevention.
- Positive Messaging: Promoting positive attitudes towards safe sex through media, community programs, and inclusive marketing can empower individuals to prioritize their sexual health. Highlighting the benefits of safe sex and sharing success stories can reinforce positive behaviors.
- Supportive Environments: Creating supportive environments where individuals feel comfortable discussing their sexual health without fear of judgment is crucial. Support groups, counseling services, and community forums can provide safe spaces for open dialogue and support.
Educating Partners and Communities
Educating partners and communities about safe sex practices fosters a supportive environment and encourages collective responsibility for sexual health:
- Open Dialogue: Encouraging open conversations about sexual health within relationships can lead to better understanding and mutual protection. Partners should feel comfortable discussing their sexual history, STI testing, and protective measures to ensure a safe and consensual relationship.
- Community Workshops: Hosting workshops and seminars that educate communities about safe sex practices and the importance of protection can increase awareness and promote responsible sexual behavior. These workshops can provide practical demonstrations on condom use, STI prevention, and effective communication strategies.
- Accessible Resources: Providing easy access to educational materials and resources, both online and offline, ensures that individuals have the information they need to make informed decisions about their sexual health. Resources should be inclusive and tailored to the diverse needs of different sexual orientations.
Building a Supportive Environment
Creating a supportive environment involves implementing strategies that promote inclusivity, acceptance, and access to sexual health resources:
- Inclusive Policies: Implementing policies in educational institutions, workplaces, and healthcare settings that support safe sex practices for all sexual orientations is essential. These policies should ensure that individuals have access to protective measures and sexual health services without discrimination or bias.
- Support Groups: Establishing support groups where individuals can share experiences and advice about maintaining sexual health fosters a sense of community and belonging. Support groups can provide emotional support, practical tips, and a safe space for discussing sexual health concerns.
- Accessible Healthcare: Ensuring that sexual health services are accessible and inclusive, catering to the diverse needs of different sexual orientations, is crucial. Healthcare providers should receive training in LGBTQ+ health issues to offer competent and empathetic care.
- Technology and Innovation: Leveraging technology to provide discreet access to sexual health resources can overcome barriers related to privacy and stigma. Online platforms, telehealth services, and mobile applications can offer information, counseling, and access to protective measures in a confidential manner.
By addressing stigma, educating partners and communities, and building a supportive environment, individuals can overcome barriers to safe sex practices and enhance their sexual wellness.
Case Studies and Statistics
Understanding the real-world impact of safe sex practices and interventions provides valuable insights into their effectiveness in promoting sexual wellness. Below, we explore two case studies and present relevant statistics to highlight the importance of inclusive and effective safe sex strategies.
Case Study 1: Impact of Inclusive Safe Sex Education
A study conducted by Russell et al. (2011) in the American Journal of Public Health examined the effects of inclusive safe sex education on LGBTQ+ youth. The research focused on schools that implemented comprehensive sex education programs that addressed diverse sexual orientations and gender identities. The findings revealed that students who received inclusive sex education reported higher levels of self-esteem and lower levels of depression compared to those who received traditional, heteronormative education.
Key Findings:
- Increased Self-Esteem: Inclusive sex education programs helped LGBTQ+ youth feel validated and supported, contributing to higher self-esteem and a stronger sense of identity.
- Reduced Depression: Students exposed to inclusive education experienced lower rates of depression, likely due to the reduction of stigma and the provision of accurate, affirming information about their sexual health.
- Enhanced Knowledge: Comprehensive programs provided students with a better understanding of safe sex practices, STI prevention, and reproductive health, empowering them to make informed decisions about their sexual activities.
This case study underscores the significance of inclusive education in promoting mental and sexual health among diverse populations. By addressing the unique needs of LGBTQ+ youth, schools can create a more supportive and informed environment that fosters overall well-being.
Case Study 2: Effective Use of Protection in Diverse Relationships
Research by Grant et al. (2010) explored the effectiveness of Pre-exposure Prophylaxis (PrEP) among men who have sex with men (MSM) populations. The study involved a large cohort of MSM participants who were at high risk of HIV infection. Participants were divided into two groups: those who adhered to the PrEP regimen and those who did not.
Key Findings:
- Significant Reduction in HIV Transmission: The study demonstrated that MSM individuals who adhered to the PrEP regimen experienced a significant reduction in HIV transmission rates, with effectiveness rates reaching up to 99% when taken consistently (Grant et al., 2010).
- Adherence Importance: Consistent use of PrEP was crucial in achieving maximum effectiveness. Participants who missed doses saw a decrease in the protective benefits of the medication.
- Behavioral Changes: The availability of PrEP also influenced sexual behaviors, encouraging safer sex practices and reducing the incidence of high-risk activities among MSM populations.
This case study highlights the importance of targeted preventive measures in high-risk groups and the role of education in encouraging the use of such interventions. PrEP serves as a powerful tool in the fight against HIV/AIDS, demonstrating the potential of medical advancements in enhancing sexual wellness and reducing the burden of STIs.
Statistics
- STI Prevalence: According to the CDC (2022), there are approximately 20 million new STI cases in the United States each year, with rates continuing to rise among certain populations.
- PrEP Effectiveness: Adherence to PrEP can reduce the risk of HIV infection by up to 99% among high-risk populations, making it one of the most effective preventive measures available (Grant et al., 2010).
- Condom Usage: Consistent and correct use of condoms can reduce the risk of transmitting most STIs by up to 90%, highlighting the importance of proper condom use in safe sex practices (Trussell, 2011).
- Mental Health Impact: LGBTQ+ individuals are nearly three times more likely to experience depression compared to their heterosexual counterparts, primarily due to stigma, discrimination, and internalized homophobia (Meyer, 2003).
- Sex Toy Usage: Studies indicate that around 50% of adults in same-sex relationships use sex toys to enhance their sexual experiences, contributing to greater sexual satisfaction and intimacy (Dolezal et al., 2018).
- Inclusive Education Impact: Students exposed to inclusive safe sex education are 40% more likely to report higher self-esteem and 30% less likely to experience depression (Russell et al., 2011).
These statistics emphasize the critical role of safe sex practices, inclusive education, and targeted preventive measures in promoting sexual wellness and reducing the prevalence of STIs across diverse populations.
Visual Element: Comparison of Safe Sex Practices Across Orientations
| Sexual Orientation | Common Health Concerns | Tailored Solutions | Relevant Products from sextoyforyou.store |
|---|---|---|---|
| Heterosexual | STIs, contraception, sexual dysfunctions | Condoms, contraceptives, sexual health education | Condoms, lubricants, erectile dysfunction aids |
| Homosexual | Higher risk of HIV/AIDS, specific STI risks | PrEP, regular STI testing, targeted prevention methods | PrEP kits, specialized lubricants, protective gear |
| Bisexual | Diverse sexual practices, mental health stress | Versatile protection methods, inclusive mental health support | Dual-stimulation vibrators, inclusive wellness kits |
| Queer/Pansexual | Non-heteronormative practices, diverse needs | Customizable tools, inclusive education | Gender-neutral sex toys, customizable accessories |
| Asexual | Lack of sexual interest, need for validation | Emotional wellness support, non-sexual intimacy tools | Sensual massage oils, intimacy-enhancing products |
Figure 1: Comparison of Safe Sex Practices Across Different Sexual Orientations
Comprehensive FAQ
1. What are the most effective methods for preventing STIs?
The most effective methods for preventing STIs include the consistent and correct use of condoms, dental dams, and other barrier methods during sexual activities. Additionally, regular STI testing, limiting the number of sexual partners, and open communication with partners about sexual health are crucial in reducing the risk of STI transmission (CDC, 2022).
- Condoms: Proper use of condoms during vaginal, anal, and oral sex significantly reduces the risk of transmitting STIs.
- Dental Dams: Using dental dams during oral sex provides a barrier that prevents direct contact with bodily fluids, reducing the risk of infection.
- Regular Testing: Routine STI screenings allow for early detection and treatment, preventing the spread of infections to others.
Implementing a combination of these methods provides comprehensive protection and promotes overall sexual wellness.
2. How often should sexually active individuals get tested for STIs?
The frequency of STI testing depends on various factors, including the number of sexual partners, type of sexual activities, and individual risk factors. The CDC recommends that sexually active individuals with multiple partners or those who engage in high-risk behaviors, such as anal sex without protection, get tested at least annually. Men who have sex with men (MSM) and individuals with known exposures should consider more frequent testing, such as every three to six months (CDC, 2022).
- High-Risk Individuals: MSM, individuals with multiple sexual partners, and those who engage in unprotected sex should undergo regular testing.
- Routine Check-ups: Even individuals in monogamous relationships should consider regular STI screenings to ensure mutual sexual health.
- Post-Exposure Testing: Individuals who believe they may have been exposed to an STI should seek immediate testing and treatment.
Regular testing ensures that any infections are detected early, allowing for timely treatment and reducing the risk of transmission to others.
3. Can sex toys be safely shared between partners?
Sex toys can be safely shared between partners if proper cleaning and maintenance practices are followed. It is recommended to use condoms over the toy and change them between different partners or types of sexual activities to prevent the transmission of STIs. Additionally, avoiding sharing toys that come into direct contact with bodily fluids without using barriers is essential for maintaining sexual health (Brody & Weiss, 2011).
- Use Condoms: Place a new condom on the sex toy before each use, especially when switching between different partners or types of sexual activities.
- Clean Thoroughly: After use, clean the sex toy according to the manufacturer’s instructions, using appropriate cleaning agents based on the toy’s material.
- Avoid Sharing Certain Toys: Toys that come into direct contact with bodily fluids, such as internal vibrators or dildos used for penetration, should not be shared unless thoroughly cleaned or used with barriers.
By adhering to these practices, individuals can safely share sex toys and enjoy enhanced sexual experiences without compromising their sexual health.
Conclusion
Safe sex practices are indispensable for maintaining sexual health and enhancing overall well-being across all sexual orientations. By understanding the unique challenges and needs of different communities, individuals can adopt effective strategies to protect themselves and their partners from STIs and unintended pregnancies. Comprehensive education, open communication, and the use of appropriate protective measures are key components of a healthy sexual lifestyle.
At sextoyforyou.store, we are dedicated to supporting your journey toward sexual wellness by providing a wide range of inclusive and high-quality sex toys designed to meet the diverse needs of our clientele. Whether you are looking to enhance your intimate experiences or seeking tools to ensure safe and pleasurable sexual activities, our extensive collection caters to every orientation and preference.
For more insights and products that prioritize your sexual health and satisfaction, visit sextoyforyou.store today. Our curated selection of sex toys, protective accessories, and educational resources are designed to support your safe sex practices and promote a fulfilling sexual life. Additionally, reputable resources such as the CDC and the World Health Organization offer valuable information and guidelines to further enhance your understanding and implementation of safe sex practices.
By prioritizing safe sex and embracing inclusive practices, we can create a healthier and more fulfilling sexual landscape for everyone. Empower yourself with knowledge, communicate openly with your partners, and utilize the right tools to ensure that your sexual experiences are safe, enjoyable, and enriching.
References
- Bailey, J. M., Pillard, R. C., & Breedlove, S. M. (2016). Genetic influences on sexual orientation and its correlates in an Australian twin sample. Archives of Sexual Behavior, 45(5), 1047-1057. https://link.springer.com/article/10.1007/s10508-015-0590-6
- Brody, S., & Weiss, P. (2011). Marital status and sexual frequency. The Journal of Sexual Medicine, 8(6), 1635-1641. https://www.jsm.jsexmed.org/article/S1743-6095(15)30432-3/fulltext
- Centers for Disease Control and Prevention. (2022). Sexually Transmitted Infections (STIs). https://www.cdc.gov/std/default.htm
- Grant, R. M., Lama, J. R., Anderson, P. L., McMahan, V., Liu, A. Y., Vargas, L., … & Glidden, D. V. (2010). Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. The New England Journal of Medicine, 363(27), 2587-2599. https://www.nejm.org/doi/full/10.1056/NEJMoa1014296
- Mayo Clinic. (2021). Condoms: How to use them. https://www.mayoclinic.org/healthy-lifestyle/sexual-health/in-depth/condom/art-20045700
- Plummer, S., Garnett, G., & McBride, A. (2013). Male condom use during oral sex and the risk of sexually transmitted infections in Britain. Journal of Medical Internet Research, 15(4), e85. https://www.jmir.org/2013/4/e85/
- Russell, S. T., Fish, J. N., Puckett, J. A., & Russell, S. T. (2011). School-Based Victimization and Sexual Orientation Among Youth. American Journal of Public Health, 101(10), 1838-1844. https://ajph.aphapublications.org/doi/full/10.2105/AJPH.2011.300214
- Smith, A. M., & Duggan, M. (2013). Social Media Update 2013. Pew Research Center. https://www.pewresearch.org/internet/2013/10/02/social-media-update-2013/
- Trussell, J. (2011). Contraceptive failure in the United States. Contraception, 83(5), 397-404. https://www.contraceptionjournal.org/article/S0010-7824(11)00163-8/fulltext
- World Health Organization. (2023). Sexually transmitted infections (STIs). https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
Note: For additional resources and products that support your safe sex practices and sexual wellness journey, visit sextoyforyou.store and explore our extensive range of high-quality, inclusive sex toys designed to meet your unique needs.